Melissa de Leon on getting breast cancer - twice

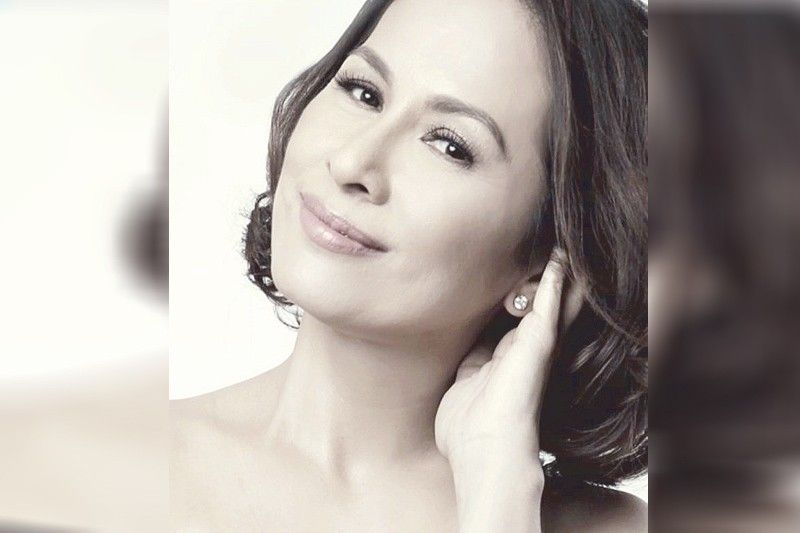
Actress Melissa de Leon discovered a lump in her left breast in 2005, a year after her long-running lunchtime show, SangLinggo Na Po Sila, on ABS-CBN ended.
“I had finished an afternoon teleserye at ABS-CBN also that same year. Thank goodness, the biopsy tested negative. Finally, I had all the time for myself and my family,” relates actress and TV host Melissa De Leon-Joseph. Or so she thought.
Little did Melissa know that a new chapter in her life was about to unfold.

Cancer scare
Melissa’s 2005 cancer scare was short-lived. In August of 2006, she had a mammogram on the same spot.
“I was asked by my doctor to have a needle biopsy, which I ignored, thinking that what the doctors had seen was just the scar from my previous operation,” shares Melissa, who went to a cancer doctor instead. The latter advised her to do the same. And the result confirmed her biggest fear.
“I was diagnosed with stage 2b breast cancer,” says Melissa, who admits she had a hard time telling her husband Ronnie and their three children — Renzo, Rigo and Rebecca — about it.
“Ronnie just hugged me in silence,” she adds. “Then we prayed.”
Melissa underwent six chemotherapies. And each session was tough.
A lot of things crossed Melissa’s mind at that time, one of which was if she only heeded her doctors’ advice early on, “it could have been stage zero.”
And so when Melissa was diagnosed with breast cancer — the second time around — in 2014, she knew better.
“It was not a metastasis,” she explains.
It’s called a second cancer. And this is different from the first cancer coming back. Women who have had breast cancer can still get other cancers, including (in Melissa’s case) a second breast cancer.
“I felt a lump in my right breast. This time I already knew that early detection could save me. So I had myself checked right away. And yes, I had my right breast mastectomy all over again,” relates Melissa, who has been cancer-free (from her first breast cancer) for 13 years now.

Early detection saves lives
Melissa is one of the resource persons in the second episode of “Tita Hope Talks: Tackling Access to Cancer Diagnosis and Navigation in the COVID-19 Era,” a timely discussion on the importance of early diagnosis in cancer care — with or without the pandemic.
An initiative by Hope from Within, a multi-stakeholder cancer advocacy campaign spearheaded by MSD in the Philippines, “Tita Hope Talks” seeks to remind the public to consult their doctor as soon as they spot something unusual and not to put off preliminary screening.
Hosted by broadcast journalist and health advocate Niña Corpus, “Tita Hope Talks” gathers experts and health stakeholders to discuss their perspective and provides their insights on various issues surrounding cancer care.
The session’s panel speakers included Dr. Beverly Ho, Disease Prevention and Control Bureau director of the Department of Health; Dr. Jorge Ignacio, Cancer Institute director of the UP-PGH; Dr. Guia Ladrera, Oncology Department section head of the Lung Center of the Philippines; Melissa Ongsue-Lee,VP for sales and marketing of Hi-Precision Diagnostics; Amiel Herrera, founder/CEO of Medcheck; and Melissa de Leon, president of breast cancer support group Project Pink.
The role of cancer screening in early detection and its impact on survival is well documented in breast, cervical, lung and colorectal cancers.
However, cancer screening has been globally interrupted by the COVID-19 pandemic. This presents oncologists with some unprecedented challenges. It is anticipated that the gap in cancer screening will result in delayed diagnoses, an increased proportion of patients presenting with advanced disease, delays in treatment, and eventually, detrimental effects on survival.

Screening: A preventive measure for cancer
Cancer detected at an early stage gives the best chance of survival. But when management is delayed, patients are more likely to face greater problems and higher costs of care.
“If cancer is in your genes, or if you have a risk for certain type of malignancy, it’s best to do regular screening,” advises Dr. Ladera. “Screening and detecting cancer at the earliest stage offers your best chance for cure.”
Compared to early diagnosis, screening is a totally different strategy that checks on illnesses that might be present, even if one is presumed healthy.
There are three Rs that need to be assed when doing cancer screening: risk factors, recommendations and rationale.
“By constantly being in check of one’s health, the effects of cancer on personal and economical aspects can be reduced,” notes Dr. Jorge Ignacio, Cancer Institute director of the UP-PGH.
Unfortunately, many patients overlook the cancer screening process due to multiple factors.
Some are worried that they might test positive for cancer, others fear the procedure itself, some are unaware of where to go and how to book a screening schedule, and to a huge chunk of patients, they view screenings and checkups as another financial burden for their families.
“The behavior that we see are usually patients have this fear of getting tested,” notes Melissa Lee, VP for sales and marketing of Hi-Precision Diagnostics. “Based on research, 50 percent of patients want to be proactive about their health, the other half would rather face the problem when it’s already there. By educating our patients about the importance of cancer screening (how it could save their lives) and that there are accessible diagnostic clinics near them, they would be more proactive with their health.”
The PGH Cancer Institute shared that pre-pandemic, the hospital would cater to an average of 120 patients daily. But in 2020 onwards, an average of 20 percent of cancer patients have not returned for their regular treatments, and some have already relapsed.
“Delaying your screening also means you could probably lose the opportunity to stop the spread of cancer,” explains Dr. Ladera. “By then, the objective of the treatment is not to cure the disease anymore, but just to prolong and improve the patient’s quality of life.”
Unlike breast cancer where one could feel a lump, the early stage of lung cancer has no symptoms except the common cough.
“That’s why most of the time, the early stages of lung cancer are accidentally found in pre-employment medical exams or pre-visa chest X-rays,” notes Dr. Ladera.
Breast cancer remains the leading cause of cancer-related deaths among women, while lung cancer is the most common and the number-one deadliest cancer among Filipino men and women.
The Department of Health offers the Breast Cancer Medicines Access Program (BCMAP) in government hospitals to support indigent cancer patients. The BCMAP aims to promote early breast cancer screening, particularly among poor women by providing assured access to medicines as well as psychosocial support.

A glimmer of hope for cancer patients
While the costs of health care in the country remains a top concern for a great number of Filipinos, MSD’s “Tita Hope Talks” sheds light on the continuous progress in providing Filipino patients better access to cancer care.
The signing of the Republic Act No. 11215, otherwise known as the National Integrated Cancer Control Act (NICCA), aims to augment cancer survivorship by strengthening essential programs throughout the whole cancer care scope.
The Cancer Law is the establishment of the Philippine Cancer Center for patients to have a ground zero for top-quality cancer treatments. And to help Filipinos with finances, a Cancer Assistance Fund is also in the works to complement the implementation of the Universal Health Care Act. It also expands PhilHealth packages for Filipinos diagnosed with cancer.
“NICCA mandates that we should have this strategic framework. And under this strategic framework are five things: good governance and sustained financing (since cancer treatment is very expensive), strategic partnerships (because the government can’t do it alone), robust information system and technologies for cutting-edge research, and capacity building and institutional strenghtening,” explains Dr. Beverly Ho, Disease Prevention and Control Bureau director, DOH.
If implemented right and funded properly, the NICCA will give better support to cancer patients, especially those from the underserved throughout every step of their cancer patient journey – from diagnosis, to getting access to treatment options, to getting post-cancer care.